MARCH 2007
I used the Peritoneal Dialysis (PD) machine overnight for a month or so. It took eight-to-nine hours every night to fully clean my blood and remove the excess fluid and toxins. Aside from alarms going off at night when the tubing kinked, things seemed to go well.
When I had to travel to Atlanta for business training, the dialysis professionals said it’s easy. The machine and fluids were shipped to the hotel, and I had to ship the machine back from hotel but keep the fluids I didn’t use. So I had to tell my two car-mates, one of whom was driving, to leave room in the trunk for several bags of fluid. Remember, we need three different dialyzate options for each treatment because weight gain differs each day. I had to borrow mailing tape from the office where I was in training because the hotel said they didn’t have mailing tape. Then I had to call in the middle of intense business training to arrange for a UPS pick-up. As I think of it, the company might not have selected the most customer-service oriented hotel. At any rate, beyond the long hours training in a new business and trying to do dialysis, the stress of returning the equipment with the limitations of a tight schedule accentuated the difficulties dialysis presents.
By doing PD overnight every day, your days are more free and you avoid going into the dialysis unit, the medical professionals said. They failed to mention the month or so of training and being stuck doing treatment every four hours until the incision where the catheter was installed adequately healed, the energy-powered machine arrived, and the patient proves comfortable determining which dialyzate fluid to use and how to track weight, blood pressure, and then add heparin, an anticoagulant that keeps the blood from clotting, to each bag of dialysate. In addition, patients must give themselves Epogen shots to promote red blood cell production.
Unfortunately, my PD failed in March. The fluid could not leave my abdomen, and I looked several months pregnant overnight. Again, this is graphic, but the nurse said if the dialysis failed, my “lips” would be full. Indeed, my genitals were swollen and disfigured. I was distraught. My façade of strength and courage crumbled, and I broke into a puddle of uncontrollable tears. I was so anxious. I cried and heaved and wondered what else could go wrong. Amy, the nurse who trained me and felt like a lifeline said she was glad to see that I was human. “What?” I was incredulous. She said I had seemed stoic through all of the diagnosis and treatment, and she wondered if I had accepted my diagnosis.
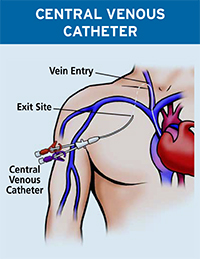
My mother drove up to take me for surgery to try to restore the failed access. Correction was not possible, so I had to go to have a catheter placed directly into my heart for hemodialysis. The surgeon left the PD catheter to be removed when I had my transplant surgery. My aunt Cheryl was still on hold for donating, and I didn’t know what was next. I can do anything for ninety days. I have said that often. But this was a change with no deadline. It meant dialysis three times per week in a unit with no expiration date. No deadline. No foreseeable end. (continued below)
Mom took me to the hemodialysis clinic, the day after it was placed in my chest near the clavicle. We sat for a while, watching people called to the back. We didn’t know what to expect or how long we were to wait. neither did we know what was behind the door techs emerged from and patients went behind. When I was finally called, Mom was not allowed in the back. I was scared–terrified might not be too strong. And Mom was beside herself. Of course she hid that for a long time. The wound was fresh, and using the catheter for treatment was painful at the incision. The dialysis nurse didn’t “realize” that the catheter was new. She was rough. I cried. I cried a lot. I think I cried through the whole treatment that first day.
If you or someone you care about is facing dialysis, please share your experiences and concerns. This is a forum for learning and inspiration. Please share your stories and questions. What were your experiences and challenges with dialysis?

I found this post very interesting. Especially some of this things you mentioned being a pain with PD. You mentioned having to choose between three strengths of dialysis fluid, or adding heparin to your bags. As a PD user myself these things are foreign to me. I only have to choose between two strengths of bags (Green 2.5% and yellow 1.5%). I have Orange 4.25% but I don’t use them to the point that I leave them at home when I travel. I also have never heard of everyone adding heparin to their bags. I assumed it was because you don’t deal with blood with PD. Maybe these things are different in different countries, as I’m Australian? Also I’m sorry your nurse was rough with your catheter, and that you have had an altogether bad experience. I hope things improve!
LikeLike
Hi Brooke,
Thank you for your input. I chose bags based on strength and had two that I used most frequently. The heparin was to reduce peritoneal fibers that can clog the catheter.
As a hemodialysis patient now, I have learned that even within the state of South Carolina the protocols are different. I have traveled to three states, and each have different practices. So I would love to have a discussion about changes in our countries!
Thank you for your follow. I am adding a new post today, and I look forward to your comments!
Blessings,
Beth
LikeLike
Yes definitely, I find it so interesting the difference in practices. Even a hospital that is only two hours away from the one I visit has different protocols regarding showering with a PD catheter. Though online reading I have a feeling that dialysis care is more strict in the USA, which can be good and bad. Pets are only discouraged while setting up and connecting, nobody wears facial masks, I can get my PD exit site wet in the shower if the water is flowing, and haemodialysis sessions always go for at least 5 hours. I always read people complaining about the 3 hour sessions, and while it is still a long time, I have to chuckle as ours go for almost double that.
LikeLike
I am so ready to go by 3 hours. some people in our unit go 6 hours, and we have a couple of nocturnal units that run 8 hours. OMG. So interesting, the differences.
LikeLike